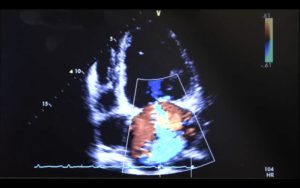
A 37 year old female presented to ED with a 9 day history of cough and dyspnoea. She had no past medical history, no foreign travel and was of Indian descent. An initial fast-track referral was made to Acute Medicine Ambulatory Care along the pulmonary embolism referral pathway. Prior to receiving any treatment the patient underwent a chest X-ray revealing significant cardiomegaly.  In lieu of these findings a bedside echocardiogram was performed by the Acute Medical team demonstrating a large pericardial effusion and engorged IVC with minimal variation. Her blood pressure remained stable and there were no clinical features of pericardial tamponade. Furthermore, M-mode on the parasternal long axis view revealed no evidence of right ventricular diastolic collapse which is typically associated with pericardial tamponade.
In lieu of these findings a bedside echocardiogram was performed by the Acute Medical team demonstrating a large pericardial effusion and engorged IVC with minimal variation. Her blood pressure remained stable and there were no clinical features of pericardial tamponade. Furthermore, M-mode on the parasternal long axis view revealed no evidence of right ventricular diastolic collapse which is typically associated with pericardial tamponade.
PLAX demonstrating significant pericardial effusion
 M-mode through PLAX showing no RV diastolic collapse
M-mode through PLAX showing no RV diastolic collapse
The patient was subsequently transferred to the Coronary Care Unit and pericardiocentesis was performed draining 1.2 litres of fluid. Cytology identified malignant cells suggesting metastatic adenocarcinoma. Unfortunately no primary source was identified for this malignancy despite extensive imaging.
A4C
Point of care ultrasound was vital in this case enabling rapid identification of significant pathology. This patient was initially referred via the PE pathway and it is plausible she may have received anticoagulation if the presence of pericardial effusion had not been identified – thus delaying intervention. Whilst pericardial tamponade primarily remains a clinical diagnosis, echocardiographic features such as diastolic RV collapse, systolic RA collapse, MV inflow variation >25% and plethoric IVC may predict an inevitable deterioration and should prompt the acute clinician to seek urgent assistance. Furthermore, were this patient to suffer a cardiac arrest, the most probable of the “4Hs & 4Ts” would become evident very rapidly. The echocardiographic features of tamponade may cause confusion to clinicians utilising POCUS on the front lines. The presence of a pericardial effusion should predominantly trigger clinicians to seek further advice/assistance and highlights the patients who may warrant some closer monitoring.