A 39 year old female presented to the Emergency Department with a two week history of worsening shortness of breath and cough. She had no past medical history with no regular medication and was eight weeks post-partum. This had been an uncomplicated pregnancy (P2G2) and normal delivery. She was initially referred to the Acute Medical Unit as a bilateral pneumonia and had been treated with IV antibiotics and IV fluids. During post-take ward round her inflammatory markers were noted to be unremarkable and further history revealed progressive orthopnoea with examination features suggesting heart failure. Chest X-ray revealed cardiomegaly, bilateral opacities and upper lobe diversion in keeping with this diagnosis. A bedside echo was performed showing severely impaired biventricular function with severe mitral regurgitation.
A bedside echo was performed showing severely impaired biventricular function with severe mitral regurgitation.
PLAX
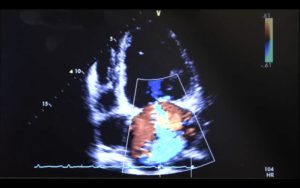
PLAX with colour doppler demonstrating MR
PSAX
A4C with colour doppler demonstrating severe MR
A4C with colour doppler demonstrating TR
 A4C CW showing MR
A4C CW showing MR
She was managed with loop-diuretics and nitrates and was referred to cardiology who commenced ACEI and B-blockers. She has been making an excellent recovery and follow up imaging has demonstrated an excellent improvement in ventricular function.